February 2024
We’ve been off to a roaring start in 2024. We have done the pre-treatment imaging ready to treat our first patient with a liver cancer on the MR-Linac. Hepatocellular carcinomas can be difficult to see on CT-based imaging but are usually very easily seen on MRI. You can read more about how we are using radiotherapy to treat these tumours on the Cancer Research UK website.
Our team members have been busy with their research outputs too. James is off to Toronto to the RTi3 conference in March to present his work on the use of diffusion-weighted MRI in patients receiving radiotherapy to a bladder cancer.

Another team member, Claire, will also be off to Toronto in May as part of the Strategic Training in Transdisciplinary Radiation Science for the 21st Century (STARS21) programme. Claire has been working hard assessing the impact that bladder filling has to the radiation dose received to the pelvis in patients with cervical cancer.
Congratulations also go to Lucy and Mark from the team. Lucy has been shortlisted for a NIHR doctoral clinical academic fellowship investigating facial asymmetry in childhood cancer survivors that have had radiotherapy treatments. Good luck to Lucy for the interviews in April!

Mark is one of our peripheral team members. He is currently undertaking a PhD at the University of Liverpool and is being co-supervised by our leader Cynthia Eccles and Rob Chuter. Mark has recently published some of his research work and it is available to read now.
Our team is expanding, and we have our first post-doctoral researcher, Rekaya. Rekaya is studying correlations between dose accumulation and clinical outcomes in the patients we have treated on our MR-Linac.

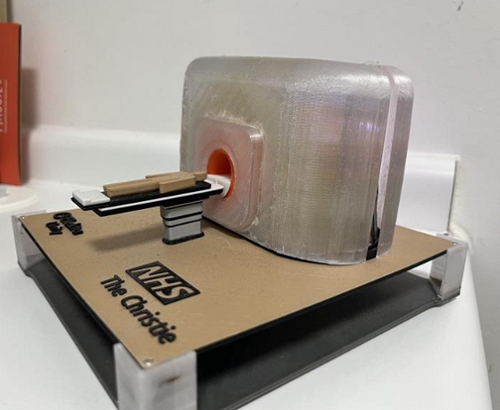
And a special thanks goes to one particular patient who made us a model of our MR-Linac!
December 2023
Autumn has been a busy time for the translational research team!
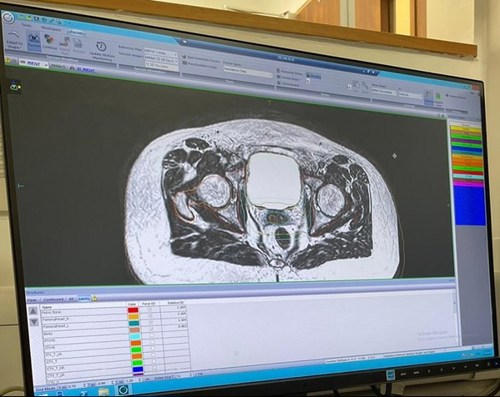
Last month, we rolled out our adapt to shape (ATS) lite workflow for prostate patients. In this workflow, the more complex ATS algorithm is utilised without the need to recontour structures. This ultimately ensures better dose conformity for organs at risk (OARs) and to the prostate.
The workflow will be further developed in the future by grouping the contours so quick adjustments can be made to account for anatomical movement. We are hoping this will increase efficiencies to treat patients allowing for a flexible but efficient planning process.
In the new year, we plan to treat our first liver patient on the MR Linac. Treatment targets in the liver can be difficult to see, particularly because the liver moves when patients breathe. Mairead Daly, radiographer and PhD student, has been doing a lot of work to reduce motion to enable better visualisation of the target. For more information on Mairead’s research, read the full article on Taylor and Francis online.
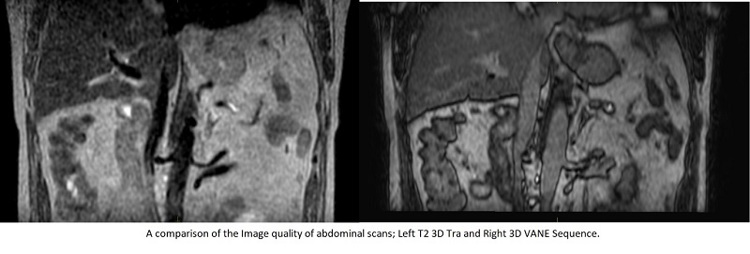
The innovation of the Phillips 3D VANE sequence, which reduces motion artefact when patients are breathing normally, and the imminent introduction of comprehensive motion management (CMM) will also support this initiative. You can read further information on the use of CMM on the Elekta website.
The MR-Linac team are active members of the Elekta MR-Linac consortium sharing our clinical progress with this worldwide group. Dr Cynthia Eccles, consultant research radiographer, is the first and only radiographer on the Elekta Clinical Steering Committee. Mairead Daly is the radiotherapy technologists (RTT) representative on the Oligomets Tumour Support Group (TSG) and Lung TSG is exclusively Christie-led by Dr David Woolf, Dr Alan McWilliam and Dr Cynthia Eccles.
Earlier in December, members of the team were subject matter experts teaching on the clinical digital oncology pathways placement for therapeutic radiography students across the country. This is an initiative led by the education team that involved 69 students. The placement allowed the students to learn about specialist areas of oncology such as brachytherapy, stereotactic radiosurgery (SRS), MR-Linac and clinical trials.
Encompassing a 2-week period, the translational research team contributed to 3 days of learning: introducing the MR-Linac, MR safety, treatment on the MR-Linac and provided 4 different anatomical case studies to apply the knowledge to. These sessions are interactive and encourage learners to complete activities, answer questions and provide feedback using digital platforms such as Slido. Our next opportunity to participate in the digital placement programme will be in January.
In October, some of our translational research radiographers, won a Greater Manchester Health and Care award for Transforming Research Delivery from the National Institute for Health and Care Research (NIHR). As the MR-Linac is a research machine, all MR-Linac patients are enrolled on a trial, and the team help coordinate all trial-related activities for our patients as well as those receiving treatment in protons and photons.

We are pleased to say that 6 radiographers have had abstracts accepted for presentation at European Society for Therapeutic Radiology and Oncology (ESTRO), Europe’s largest interdisciplinary radiotherapy congress. We will also be giving an invited educational talk by Dr Cynthia Eccles. There will also be plenty of Christie MR-Linac presentations from our colleagues in physics, clinical oncology, and academia.
Radiographers from the photon departments have also been successful having abstracts accepted. Please see below a list of all works being presented in Glasgow this year.
|
Name of abstract author |
Abstract name |
Format of abstract |
|---|---|---|
|
Phil FendallAmaro |
Radiographer led feasibility trial of remote cardiac monitoring post radical thoracic radiotherapy |
Digital poster |
|
Lee Whiteside |
Accessibility of clinical research: A retrospective analysis of clinical trial patient demographics within a large UK radiotherapy centre |
Digital poster |
|
Mairead Daly |
Evaluation of accumulated OAR dose DIR methods for MR-guided pancreas SABR |
Poster discussion |
|
Mairead Daly |
Implementation of RTT-led OAR delineation training for pancreatic SABR on the MR Linac |
Poster discussion |
|
Mairead Daly |
Effect of motion management strategy on interobserver delineation variation in MR-guided abdominal radiotherapy |
Digital poster |
|
Mairead Daly |
Patient-specific factors impacting free-breathing motion magnitude and variability on MRI for radiotherapy |
Proffered paper (presented by Holly Egan) |
|
Lisa McDaid |
Prostate SABR radiotherapy on the MR-Linac: how can we improve service efficiency? |
Digital poster |
|
Amerah Alshamrani |
Adaptive strategies for external beam radiotherapy in cervical cancer: a systematic review |
Poster discussion |
|
Rachael Bailey |
To what extent does proton imaging training enhance confidence in reviewing proton plan |
Poster discussion |
|
John Rodgers |
Off with their heads! A comparison between 4- and 5-point immobilisation for thoracic patients |
Digital poster (presented by Rhianne Kelly) |
|
John Rodgers |
The tortoise or the hare? Evaluation of an accelerated CBCT imaging preset in thoracic IGRT |
Digital poster (presented by Lydia Dearing and Dylan Collins) |
|
Cynthia Eccles |
The use of MRI-guided palliative radiotherapy for metastatic spinal cord compression |
Invited educational talk |
July 2023
New Paterson cancer research centre
After the fire that caused severe damage to our Paterson research building 6 years ago, the new £150m cancer research centre has now opened. The Christie, Cancer Research UK and The University of Manchester are the 3 partners who will call the building at The Christie’s site on Wilmslow Road in Withington home.
The new research centre will be one of the world’s leading cancer research facilities. It will house over 700 multidisciplinary experts working in collaboration on clinical trials covering the full extent of the patient pathway, from prevention and novel treatments to living with and beyond cancer. The aim is to double the number of patients in clinical trials by 2030, and ultimately improve outcomes and survival rates. Our translational radiotherapy research team will play a key role in the evolution of radiotherapy research and will have access to the state-of-the-art facilities provided.

You can see a video timelapse of the building being built on our YouTube channel.
Implementation of radiographer-led organ at risk (OAR) delineation for pancreatic SABR
We are excited to announce the roll-out of online radiographer-led OAR contouring for pancreatic SABR on the MR-Linac!
Undertaken within a research framework, lead by PhD student Mairead Daly, this cutting-edge approach empowers skilled radiographers to enhance precision and consistency in critical structure delineation, optimising treatment planning for better patient outcomes. Proud to be part of this transformative leap in radiation therapy!
Spotlight on the physics team
This month, our Spotlight on… series focuses on our physics team. These team members do a lot of work behind the scenes that patients may not be aware of. Our clinical scientists are integral members of our hard working, dedicated radiotherapy team.
Clinical scientists undertake monitoring and checks to ensure that MR-Linac is safe and ready for scans and treatment. Other vital roles include treatment planning, quality assurance, and work with the interdisciplinary team providing advice and support.
Radiotherapy clinical scientists are also part of the team present during treatment delivery and are closely involved in the adaptive re-planning patients’ treatment. Additionally, clinical scientists undertake local commissioning of new technologies and techniques and are essential to the design and delivery of radiotherapy related research.
MRI clinical scientists work to ensure that the integrity of the imaging components of the MR Linac are safe and accurate. They develop or optimise, and develop new imaging sequences for treatment and for exciting new radiotherapy trials. Both the radiotherapy and the MR clinical scientists represent The Christie at national and international conferences.
Working in the MR-Linac team at The Christie
The Christie MR-Linac team is currently recruiting for a specialist therapeutic research radiographer in clinical trials and research.
Please contact Cynthia Eccles at cynthia.eccles1@nhs.net if you want more information on either role.
May/June 2023
Spotlight on the observations team
A multidisciplinary team is essential for the day-to-day running of the MR-Linac, with plenty of work going on behind the scenes. Our new Spotlight on… section will give other teams the chance to introduce themselves highlighting their role within the patient pathway.
In this month’s blog, we would like to acknowledge the work that is also done by the observational and supportive research team for trials on the MR-Linac, such as the MOMENTUM and MR-BIO study.
I’m Anthony Murphy, a research nurse working in the research team alongside Suzanne Allibone, senior research nurse.
Recently, we have faced some challenges including staffing capacity and the COVID-19 pandemic. These challenges saw studies like Momentum and MR-BIO paused for a time.
However, we are pleased to announce as well as working together with the MR-Linac radiographers, we now have 2 new members in our team. These are Rachel Campsey, an experienced research nurse who has worked at The Christie for many years including working with the rare tumours team, protons and more recently at the Maggie’s centre. We also welcome Chloe Newton in a new role within the team as a senior clinical research practitioner. Chloe has previously completed her Masters in breast cancer research and worked as a research practitioner at Wythenshawe Hospital. A warm welcome to them both.
Since recruiting our first patient on the MOMENTUM study at the end of 2019, the research team have successfully consented and recruited 204 imaging and treatment participants and 54 imaging-only participants. These are across 7 disease groups including prostate, bladder, pancreas, cervix, head and neck, lung and other. We also collect data from these patients, with questionnaires and toxicity assessments performed at various time points including baseline, 3, 6, 12 and 24 months.
The MR-BIO study has also recruited 55 patients. This includes the research nurses co-ordinating numerous visits for trial blood and urine sample collections.
The observational and supportive research team are continuing to work hard on these studies and are more than happy to be contacted about any of these observational studies. I would also like to thank the MR-Linac radiographers who, over the last few years, have helped in covering consents when the observational team have been unavailable.
The observational supportive research team can be contacted on email: OSRT@christie.nhs.uk
Recent MR-Linac highlights
Clinical work continues on the MR-Linac, and beyond. Here are some of the highlights from the past months.
The European Society for Radiation and Oncology (ESTRO) conference took place in Vienna in May and was a resounding success for our team members (see blog by Ben Dobby – April 2023). MRL team members authored or co-authored the below listed MR-Linac-related conference papers:
- Quantifying the benefits of online daily adaptation for MR-guided RT in cervical cancer
A. Alshamrani, A. Choudhury, C. Eccles, M. Aznar, R. Chuter, P. Hoskin - Evaluation of patient positioning for accelerated partial breast irradiation on an MR-Linac
Davies, L. McDaid, C. Anandadas, L. Whiteside, A. Clough, R. Benson, P. Fendall Amaro, J. Parker, H. Drury-Smith, C. Eccles - Evaluation of intrafraction duodenum positional stability for pancreatic SABR on the MR-Linac
Daly, A. Choudhury, R. Chuter, B. Erickson, W. Hall, A. McWilliam, E. Vasquez Osorio, G. Radhakrishna, H. Verkooijen, C. Eccles - Automated analysis of internal facial asymmetry on MRI in children
Davey, A. Bryce-Atkinson, E. Vasquez Osorio, M. van Herk, A. Datta, S. Pan, P. Sitch, G. Whitfield, M. Aznar - Impact of advancing radiographer practice on MRL treatment times
Clough, R. Benson, C. Nelder, L. McDaid, L. Freear, R. Chuter, J. Berresford, C. Eccles - Incidental findings in non-patient, volunteer MR imaging: a single centre experience
McDaid, A. Datta, J. O'Connor, P. Manoharan, S. Bonington, A. Choudhury, P. Hoskin, R. Huddart, C. Eccles - Optimising the MRL Consortium Biomarkers Group Prostate DWI Sequence Image Quality & ADC Comparison
Moore, A. Clough, C. Nelder, C. Eccles, P. Hoskin, R. Chuter, J. Zhong, D. McHugh, A. Choudhury, M. Dubec - Does the presence of Magtrace preclude adaptive breast radiotherapy on an MR-Linac?
Davies, L. McDaid, C. Anandadas, P. Fendall Amaro, R. Chuter, D. Woolf, C. Eccles
Work will now continue towards publishing full manuscripts and preparing new work for next year’s closing date, which is fast approaching!
The annual Christie Advanced Radiotherapy Summer School took place from 27 to 29 June 2023. The interactive 3-day course covers a variety of hot topics in radiotherapy.
Day 2 focused on MRI-guided and adapted radiotherapy and included talks by Prof Peter Hoskin on MR guided radiotherapy, Michael Dubec (clinical scientist in MRI Physics and PhD Candidate) on optimising MR for Radiotherapy, Dr Cynthia Eccles on the clinical applications for functional MR and Linnea Freear (clinical scientist in radiotherapy physics) integrating MR in to radiotherapy workflow to a diverse audience consisting of a wide range of professionals.
We would also like to thank our colleagues from proton beam therapy, David Lines and Rachael Bailey for a lively debate with Frank Brewster and Cynthia Eccles on which technology is better (clearly MR-Linac)!
A special mention to Michael Dubec
The 18th annual MR-Linac Consortium took place in Amsterdam in June. We are pleased to share Michael Dubec, Clinical Scientist MRI was awarded best technical abstract for his work on oxygen enhanced MRI (see blog by Ben Dobby – April 2023). This work has made positive steps towards biologically-guided radiotherapy.
The new Paterson building is now open! Next month, we will introduce you to the building and explain how it will be one of the world’s leading cancer research facilities.
April 2023
Prof van Herk on the MR-Linac and other ways to improve radiotherapy
Before joining The Christie as Chair in Radiotherapy Physics, Professor Marcel Van Herk was an established leader in his field and a world expert in using image guidance systems for radiotherapy. His work over the last 30 years, including the Van Herk formula, has helped millions of people benefit from more effective radiotherapy.
Here, Professor Van Herk explains how he’s using the MR-Linac in his research to help make new ground-breaking cancer discoveries.

What’s the focus of your research at The Christie?
All of the work I do is about making radiotherapy treatment more precise. The more precisely you can hit a tumour, the less healthy tissue you hit. Which means better outcomes for patients. For example, we’ve recently discovered that the top part of the heart is particularly sensitive to radiotherapy. So we now know we must avoid this particular area when delivering the treatment to lung cancer patients.
Since I moved to Manchester, my group has expanded to 3 senior lecturers, 4 postdocs, and 17 PhD students. As ever, our group is keen to improve precision of radiotherapy. This work follows several avenues.
The main focus of the group is to learn from every patient treated. We look at how thousands of patients were treated in the past and relate the outcomes to detailed information of their treatment.
Since 2017, we have a fantastic infrastructure (and appropriate governance) in place allowing use to research data of all patients treated in The Christie – unless opted out. Next month, we will introduce heart-sparing lung cancer radiotherapy as direct consequence of this work, in what we call rapid learning trial.
As of mid-March, all patients will receive the newly optimised treatment, using routine data collection to confirm that the new treatment is indeed better. Several researchers are looking at practical, ethical, statistical, and data collection aspects in an MRC grant.
In the CRUK-funded RADNET project, we study what other diseases patients may have next to their cancer and see how these interact with the cancer and their treatment, with an ultimate aim to personalise radiotherapy to each patient’s circumstance. For instance, we are exploring the effects of muscle mass, sarcopenia.
Then, we work to optimally utilise the equipment. 2 of my PhD students are exploring how the amount of imaging dose in image guided radiotherapy for children and adults can be reduced without loss of information. Their recommendations are likely to change clinical practice.
How are you working on improving the precision of radiation?
In the past, the problem with radiotherapy was that you couldn’t always see what you needed to hit. But the new MR-Linac (radiotherapy with an MRI scanner for image guidance), which Christie supporters helped to fund, can give us the very best image guidance for delivering radiotherapy thanks to the superior image quality of MRI. Now we need to develop the systems that make the best use of this technology for everyday treatment.
After introducing the MR-Linac for routine care, focusing on tumours that are difficult to see on CT, we are now exploring new possibilities. The MR-Linac offers unique possibilities to study patients’ biological response to radiotherapy.
Our MRI group (recently grown to 5 members) is now actively developing and applying so-called oxygen enhanced imaging. This technique measures the oxygen consumption of tumour and healthy tissues, which is important factor in tumour control and toxicities.
A new allied health professional academy has 5 radiographer PhD students optimising the delivery side of things, with as aim to perform a clinical trial of biology-adapted radiotherapy within the next 5 years.
What is the Van Herk Formula?
This is the formula to work out the proper safety margin to treat a patient – it should be big enough to safely cover the entire tumour with a high dose, but small enough to avoid giving too much dose to the healthy tissues in each patient.
Uncertainties in radiotherapy continue to have my interest. We have explored anatomical changes in lung, cervix, and head and neck cancer patients, and use this information to predict when best to intervene in routine treatment or to select patients to get the best treatment on the different treatment machines the Christie has.
What do you hope to achieve next at The Christie?
It’s all about precision and personalisation, so trying to make the treatment and equipment optimised for every patient that comes through the door.
This remains my long-term goal, and we have managed to make steps to start make this vision a clinical reality.
To ensure we can keep making breakthroughs in cancer treatments, The Christie Charity is running a campaign to raise funds for cancer research. A donation from you today can help fund the research to bring the next breakthrough into focus.
MR-Linac update – April 2023
It has been all things go here on the MR-Linac! We have been working hard to get our new team up to speed, pursuing further education, focusing on our individual research projects so that we can welcome more and more patients through our doors.
In the first quarter of the year, we have recruited 37 patients and healthy volunteers to trials for treatment and imaging on the MR-Linac. Alice is now supporting or leading the co-ordination of MR-Linac-based trials including PRIMER, MINION, BIOCHECC, HYPROGEN, QUANTUM, CPAP and RO-PIP. The observational team continue to co-ordinate for MOMENTUM and MRBIO and we are very glad for their support.

The team have taken on a new professional development opportunity from the University of Alberta. This course has focused on MR safety, spin physics, image contrast and much, much more. Although challenging, it has been an interesting topic, and everyone has passed with flying colours!
Cynthia (consultant research radiographer) and Lisa (principal radiographer) contributed as subject matter experts: with Cynthia being the curriculum content advisor and then auditing the course with others prior to it going live. It is the first CPD offering of its kind in Canada and the 2nd cohort it has been run in. The team has taken a lot from this course and are now implementing this knowledge into our day-to-day operations on the MR-Linac.

The European Society for Radiation and Oncology (ESTRO) conference is just around the corner. 4 members of our team have had their proposals accepted and are now fine tuning their projects in preparation of this upcoming event.
List of projects
- Lisa McDaid: ‘Incidental findings in non-patient volunteer MR imaging: a single centre experience’
- Lucy Davies: ‘Does the presence of a mag trace preclude adaptive breast radiotherapy on an MR-Linac’ and ‘Evaluation of patient positioning for accelerated partial breast irradiation on an MR-Linac’
- Mairead Daly: 'Evaluation of intrafraction duodenum positional stability for pancreatic SABR on the MR-Linac'
- Abbie Clough: ‘Impact of advancing radiographer practice on MR-Linac treatment times’
Travel arrangements are now in place for their journey across to Vienna! We wish them all the best of luck and look forward to sharing their work in a future blog.
In other news, our team has new published work! Michael Dubec, clinical scientist (MRI) and PhD student (who we work closely with) and his supervisor Professor James O’Connor have published “First-in-human technique translation of oxygen-enhanced MRI to MR-Linac system in patients with head and neck cancer”. Thank you to all the participants who allowed us to scan you on the MR-Linac for this very important work. The paper can be found on thegreenjournal.com.
In a final update for this month, we modified the MR-Linac bunker last year so that patients undergoing treatment and imaging would be able to breath pure oxygen. This has allowed us to study oxygen-enhanced MRI – a method of acquiring repeat images over a period where the participant first breaths medical air, then pure oxygen and then is switched back to medical air again.
In doing this, we can see changes in the region being imaged that take up or reject oxygen uptake. These areas that do not take up oxygen are called ‘hypoxic’. Some cancers are entirely hypoxic or have hypoxic sub-regions. These areas can be resistant to radiotherapy and other cancer treatments. This work is an important first step in learning where and when these hypoxic regions develop so that we can better learn how to improve treatment to them.
Next month, we will introduce you to some of the other teams behind the scenes at the MR-Linac and associated research.
January 2023
We’re back! After a longer than expected hiatus, we are back to blogging about the MR-Linac at The Christie.
And there has been a lot of change on the MR-Linac since the last blog post. Firstly, a few members of the team have moved to different roles and there are 3 new radiographers – Jay, Ben and Alice.
Jay, an avid reader and football enthusiast has joined us after previously working on an MR-Linac in the private sector and at the Royal Marsden. Ben has moved across from the treatment floor here in radiotherapy and when not at work, he likes to try his hand at DIY. Alice, who most recently worked at the new Christie at Macclesfield centre, unwinds with crochet and hiking in her spare time. All 3 are bringing a wealth of experience and are assets to the team, helping to improve the service and patient experience.

Moving onto the technical news, we have expanded the patient cohorts we treat on the MR-Linac. In May 2022, we treated our first patient with pancreatic cancer. These tumours can be difficult to see with the conebeam CT (CBCT). Using MR imaging we can better visualise target improve treatment accuracy. Using our Adapt to Shape (ATS) online re-planning, the interdisciplinary team can re-contour the position of organs close to the tumour daily and then plan the treatment according to that position.
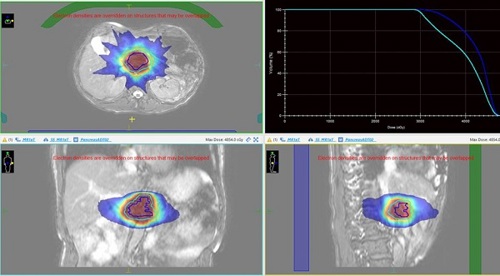
Below is a picture of a treatment plan for a patient with a pancreas tumour. Note the high dose region in the red colourwash, covering the target (plus a margin for breathing motion) in the blue and cyan lines.
Bladder patients are another cohort we are treating and with the installation of the piped oxygen we can connect carbogen gas. The administration of carbogen and nicotinamide (BCON) during radiotherapy is a treatment regime that was developed at Mount Vernon hospital as an alternative for patients with bladder cancers, for whom chemotherapy would be considered too aggressive. The patient breathes high flow oxygen (carbogen) whilst receiving radiotherapy treatment this oxygenates tumour cells to make them more sensitive to radiotherapy. We can combine this with treatment on the MR-Linac, where the patients’ bladder and nearby organs can be re-contoured daily to improve treatment accuracy.
We have also started Oxygen Enhanced MR imaging (OEMRI), a technique that visualises the oxygen uptake in cells in the body by getting patients to inhale oxygen whilst being imaged. This highlights areas that have poor oxygenation. 3 trials using this technique are OE H and N, recruiting patients and volunteers to help develop head and neck imaging, Bio-CHECC, which focuses on patients with locally advanced cervical cancer and Hyprogen, imaging patients with advanced prostate cancer. This is exciting as it has the potential to give us additional information about treatment response in (near) real-time and the prognosis of certain tumours.

During 2022, we recruited 131 patients across 6 MR-Linac specific research studies and we are hoping that 2023 is just as or even more successful.
Our team are constantly hard at work with developing new techniques and opening new research studies – there are a lot more updates to come!
October 2021
Our first MR-Linac head and neck cancer patient
We have now treated our first head and neck cancer patient on the MR-Linac.
Bob from Whitefield completed 20 fractions of head and neck radiotherapy on the MR-Linac in October 2021. Under the care of Dr Andrew McPartlin, Bob has coped very well throughout his treatment.
As well as receiving support from his clinical team, Bob was also supported during his treatment by his 2 sons. One of his sons lives near him and one lives in Spain and came over to help him while he was having his treatment.
Being able to treat more patients with different types of cancer is very exciting for the whole multidisciplinary team on the MR-Linac. It means we can deliver more targeted radiotherapy for more patients, and deliver more personalised care with kinder treatments.

July 2021
New endeavours and exciting times
Over the past few months, it’s been all things new here on the MR-Linac. Firstly, we have 2 new members of our clinical trials team – Philip Teles Amaro and David Roberts. Both will be valuable assets, helping to deliver treatment, conduct scans and further enhance the patient experience on our MR-Linac.
We have also had some new equipment delivered. The Bayer-Medrad™ contrast injector now installed on our Unity MR-Linac is believed to be a world first. The contrast injector will allow the radiotherapy team to administer contrast agent to further enhance our scans, and potentially future treatments. We have also had a gas panel installed to allow treatments under general anaesthetic, and our team are working on the development of oxygen-enhanced images for the MR-Linac – this could change how we treat patients in the future.

We’re also starting to treat new groups of patients on our MR-Linac. In January 2021, we started treating prostate patients under the PACE-C trial. This means we can now treat patients with intermediate to high-risk prostate cancer.
After much complex work in the background, we have also started treatment of our first patient with lung cancer. The potential benefits we could provide to this patient group with adaptive radiotherapy is very exciting for our whole multidisciplinary team.
As the indication list for our MR-Linac grows, we’re able to treat patients with increasingly complex cancers in more difficult locations. We’ve started identifying our first patient with oropharyngeal cancer for treatment.
Our busy team have also helped expand the knowledge base of the MR-Linac, with assistance in new research publications including Lee Whiteside “Development and results of a patient-reported treatment experience questionnaire on a 1.5T MR-Linac” and Claire Nelder “Adaptive Radiotherapy in the Management of Cervical Cancer: Review of strategies and clinical implementation”.
Outside of work, our MR-Linac team are currently competing in the “Miles for radiotherapy” challenge to help raise awareness of the cause and raise some money for charity.
Stay tuned for more exciting news from the world of the MR-Linac over the next few weeks.
February 2021
This month, we introduced adaptive fractionated cervical radiotherapy on the MR-Linac. This made us the first site in the Elekta MR-Linac consortium to do so!
To coincide with cervical cancer awareness week in the UK, the MR-Linac team completed the MR simulation. We did this with a view to treating our first patient with cervical cancer fully on the MR-Linac – this would be 25 fractions.
We have been preparing for this and searching for someone suitable to treat for quite some time. But now the day is here!
Our simulation scans took place on 18 January, followed by a day 0 mock treatment with the full team present to ensure everything would run smoothly on 29 January. After this, treatment began in earnest on Monday 1 February.

How did we get there?
Lots of hard work goes on behind the scenes, in order to ensure new treatment sites are treated safely and accurately.
Let us walk you through the process…
Optimising images
To start with, we need to make sure the MRI scans from the MR-Linac are fit for purpose. In this case, ‘fit for purpose’ means the scans define the areas to be treated or avoided. It also means we can use them to match each daily treatment to assess whether or not adaptation is required to account for anatomical or physiological changes.
Before we can do this for real treatments, our radiographers acquire MR images from volunteers taking part in the PRIMER and MOMENTUM studies. The radiographers and doctors then assess the scans to see if these images work for treatment with our team of physicists, testing new imaging sequences until they are treatment ready.
The PRIMER and MOMENTUM trials are data collection studies, investigating clinical and technical data of patients having treatment on the MR-Linac. The data is used for service development, and consequently implementation of the best evidence based practice on the MR-Linac.
Contouring workshop
We recently held a workshop so our radiographers, physicists and doctors could prepare for day 0, using the contouring tools on Monaco (our computer planning system).
For our cervix treatment, one of the doctors will contour the patient’s anatomy on a daily basis using the ‘adapt to shape’ (ATS) planning system.
As organs within the body move during the course of a radiotherapy treatment, the ATS software will allow us to adapt the plan to the patient’s anatomy daily. This means we can improve treatment accuracy and lower the dose to the surrounding healthy tissues.
Day 1 treatment
The focus and determination of our interdisciplinary team for the last few years has all been worth it. We successfully treated our first fraction of radiotherapy for a cervix patient, adding to the treatment sites commandeered by the MR-Linac.
Stay tuned for our next blog to see what is next on the horizon.
