What is spinal cord compression?
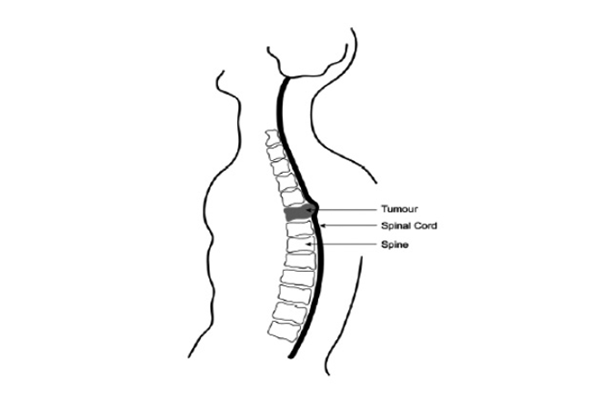
The spinal cord is the large bundle of nerves that runs from the brain to the bottom of the back. The bones of the spine (vertebrae) protect it. As it passes through each bone, the spinal cord gives off smaller nerves called nerve roots. These supply the trunk, arms and legs with sensation (feeling), and control of muscles. This includes control of the bladder and bowel.
Spinal cord compression is pressure on the spinal cord and its nerves. This may happen because:
- the bones are affected by cancer,
- a secondary tumour is damaging the vertebra, or
- the cancer has spread to tissues around the spine.
What are the symptoms of spinal cord compression?
This depends on the part of the spinal cord affected by the tumour, and may include:
- an ache in your neck or back or in the area supplied by the nerve roots (spreading around the side of your body or down your arms or legs)
- nerve pain, sometimes described as burning or shooting
- some change in sensation and strength in your legs, or arms and legs
- not being able to empty your bladder, or
- loss of control of your bowel and your bladder.
Your care
- All patients with suspected spinal cord compression will need to have a special scan of the spine, usually an MRI scan. This is to show exactly where the spine and nerves are affected. It will also help us to make decisions about the best treatment.
- You will need to rest flat in bed, as sudden movement of the spine may make things worse. You will be given nursing care to keep you comfortable while you are in bed. You will need to stay flat at least until you have had a scan. If the scan shows that the tumour is making your spine unstable you will need to stay flat until it has been stabilised.
- You will be given help with bladder/bowel care if you need it. You may need a catheter to help empty your bladder.
- A hard collar may be provided to support your neck (if your neck is involved).
- Steroids (dexamethasone) are usually given to reduce inflammation and swelling around nerves. If you are diabetic, or have had problems with steroids in the past, please tell your doctors. The steroids will be gradually reduced after you have had treatment.
What is the treatment for spinal cord compression?
Radiotherapy is the usual treatment for spinal cord compression, this uses high energy rays to shrink the spinal tumour. The aim is to take pressure off the spinal cord. An operation may be suitable for some patients. Your medical team will provide more details about this if appropriate.
What are the benefits of radiotherapy?
Radiotherapy will improve your symptoms and help to relieve the pain. Sometimes it can stop the weakness from becoming worse. Unfortunately, there is not a good result in all cases especially if the nerve damage is severe and there is no movement in the limbs at all. It can take 2 to 4 weeks after radiotherapy to get an improvement in symptoms.
The return of some strength or sensation in the first week is an encouraging sign. No change at all in the first week means that recovery is unlikely.
Are there any alternatives to radiotherapy?
Surgery and radiotherapy can be used to treat the affected part of the spine. Specialist teams will look at your scans and discuss the best treatment for you. If surgery seems to be a better option than radiotherapy, this will be discussed with you. However, many patients with cord compression will not be suitable for an operation.
For patients with some tumours, such as lymphoma, the initial treatment is likely to be chemotherapy. You will be given further information about the treatment you are advised to have once the results of your scan are known.
What happens if I decide not to have any treatment?
Spinal cord compression is a serious condition that needs immediate treatment. If left untreated it could lead to permanent damage and paralysis.
What happens if I have radiotherapy treatment?
Before treatment can begin, we have to plan the treatment using information from the scans. You will lie on your back under a special machine called a ‘simulator’ or a CT scanner. Measurements are taken and marks are drawn on the skin over the area to be treated.
One tiny permanent mark is made on your skin, so that you can be set up in exactly the same position at treatment. These marks can be used if you have radiotherapy in the same area in the future. You will have the treatment on a different machine called a linear accelerator.
You lie on a couch in the same position as you were scanned in. Treatment takes just a few minutes and it is painless. Some people have several treatments, although usually it will be given in one session. Your oncologist will explain the treatment plan to you.
Are there any side effects?
Side effects are not usually a problem but these depend on the area to be treated. For example, treatment to the neck may cause a sore throat but this will usually not develop until a week or two after treatment.
Treatment to the upper spine (chest area) may inflame the gullet and cause temporary soreness on swallowing, again not until the week after. Sometimes treatment can cause a pain flare, and if the lower spine is treated, it may cause diarrhoea, nausea and sickness, although this is not common. This can often be prevented by an anti-sickness tablet at the time of treatment. Any sickness happens only in the first 24 hours after radiotherapy.
What happens after treatment?
Patients with spinal cord compression are likely to be nursed flat in bed at first. The medical and physiotherapy team will assess you and plan how to get you mobile as soon after treatment as possible. This will be done carefully. If this causes pain or worsening of the nerve symptoms, we will take the process more gradually.
If there is some movement in your limbs you will be taught useful exercises for you to do in bed to improve muscle tone and build up strength. The physiotherapists and occupational therapist will assess you and will advise on equipment that might be needed to help you with activities and to become as mobile as possible.
During this time, the team will be talking to you and your family about the likely recovery following treatment and helping to plan further care. If you are unable to manage at home, you may need to transfer to a different hospital. If it is possible to help you make further improvements in mobility and function, we may suggest further care (rehabilitation). However, not everyone may benefit from this.
The steroids will be gradually reduced after your radiotherapy treatment. The staff know that this can be a very difficult and worrying time for you. A number of people are there to help:
- acute oncology teams are based in all hospitals and are there to support you
- complementary therapists, who can provide care such as massage of the legs, relaxation or aromatherapy
- the palliative care team, who may be able to advise on pain control, other symptoms and to support you and your family
- the social work team who can help you look at different options for ongoing care, if you need it
- the complex discharge team, who will co-ordinate plans for your discharge
- counsellors who will support you to cope with how you are feeling about what has happened to you.
Useful contact numbers
- Macmillan Cancer Support
Freephone helpline: 0808 808 00 00
Mon to Fri, 9am to 8pm
www.macmillan.org.uk
